70 Years old male weaver by occupation came to hospital for his maintainence hemodialysis .
Patient was apparantly asymptomatic 1 1/2 month ago then he developed fever which is sudden in onset high grade associated with body pains, headache and burning micturition for which he went to local RMP and took some medications and the fever is relieving on taking medication ,it is not associated with cold, cough, sorethroat, nausea, vomitings after 10 days patient developed swelling in both legs up to knee which is insidious in onset gradually progressive , pitting type no aggrevating and relieving factors . He also had facial puffiness which is more in the morning . Patient also had loss of appetite and decreased urine output for which he went to a local hospital there he was given some medication and he used them for around 8 - 10 days but his symptoms were not subsided. Then he came to our casuality with the complaints of loss of appetite, nausea, burning micturition and reduced urine output and here he was diagnosed with CKD and HYPERTENSION. He was kept on dialysis. 4 sessions of dialysis were done and later patient went home and came to the hospital 4 days ago for his maintainence dialysis after the dialysis patient developed shortness of breath and low BP so he was shifted to ICU and patient was started on oxygen and Noradrenaline infusion (10 ml/hr) few hours later patient became stable. Later, paient has 2 episodes of vomiting which was non projectile, black color , contents bening some food particles.
PAST HISTORY
No similar complaints in the past.
No H/o DM, TB, ASTHMA, EPILEPSY.
Patient has a history of cataract surgery for both 6 years ago.
PERSONAL HISTORY
DIET - Mixed
APPETIE - Decreased since one month
SLEEP - Adequate
BOWEL MOVEMENTS - regular
ADDICTIONS - Patient has history of smoking since 50 years and smokes 20 beedis per day.
He also has history of alcohol consumption since 40 years and consumes around 40-50 ml per day.
FAMILY HISTORY
No H/O similar complaints in the family.
ALLERGIC HISTORY
No known drug and food allergies.
GENERAL EXAMINATION
Patient is C/C/C
VITALS
TEMP: afebile
BP : 110/70 ON NORADRENALINE 10 ML / HR
PR :118 BPM
SPO2 : 98%
PALLOR +
NO EVIDENCE OF ICTERUS, CYANOSIS, CLUBBING, LYMPHADENOPATHY.
Black coloured vomitus
SYSTEMIC EXAMINATION
CVS - S1, S2 heard and no murmurs
RS - BAE + , No added sounds
P/A : Soft , No tender, no evidence of organomegaly.
CNS : No Focal neurological deficits.
Provisional Diagnosis
? CKD ON MHD WITH SEPSIS
? HYPOVOLEMIC SHOCK SECONDARY TO UPPER GI BLEED.
HEMATESIS UNDER EVALUATION (? UREMIC PLATELET DYSFUNCTION
? PEPTIC ULCER DISEASE )
EVENTS TIME LINE UPTO 7/8/21
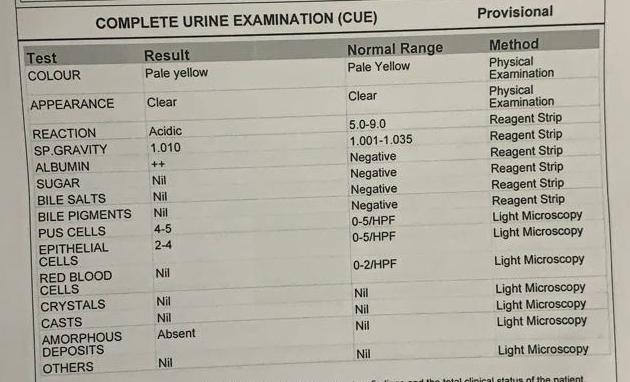
INVESTIGATIONS
4/10/21
Serology - Negative
CBP
TREATMENT GIVEN
- Inj. PANTOPRAZOLE 50 mg in 500 ml NS Iv over 2-3 hours
- Inj. TRANEXA 1ampoule Iv stat
- Inj. Vit K one 1 ampoule Iv stat.





















Comments
Post a Comment